Overcoming barriers thanks to pediatric therapy
Zachary bounces into the room, bright-eyed and ready to dive into a session with his occupational therapist, Ashley Miller. She tells Zachary that she likes his red shirt and he excitedly shares that it’s red because it’s Valentine’s Day.
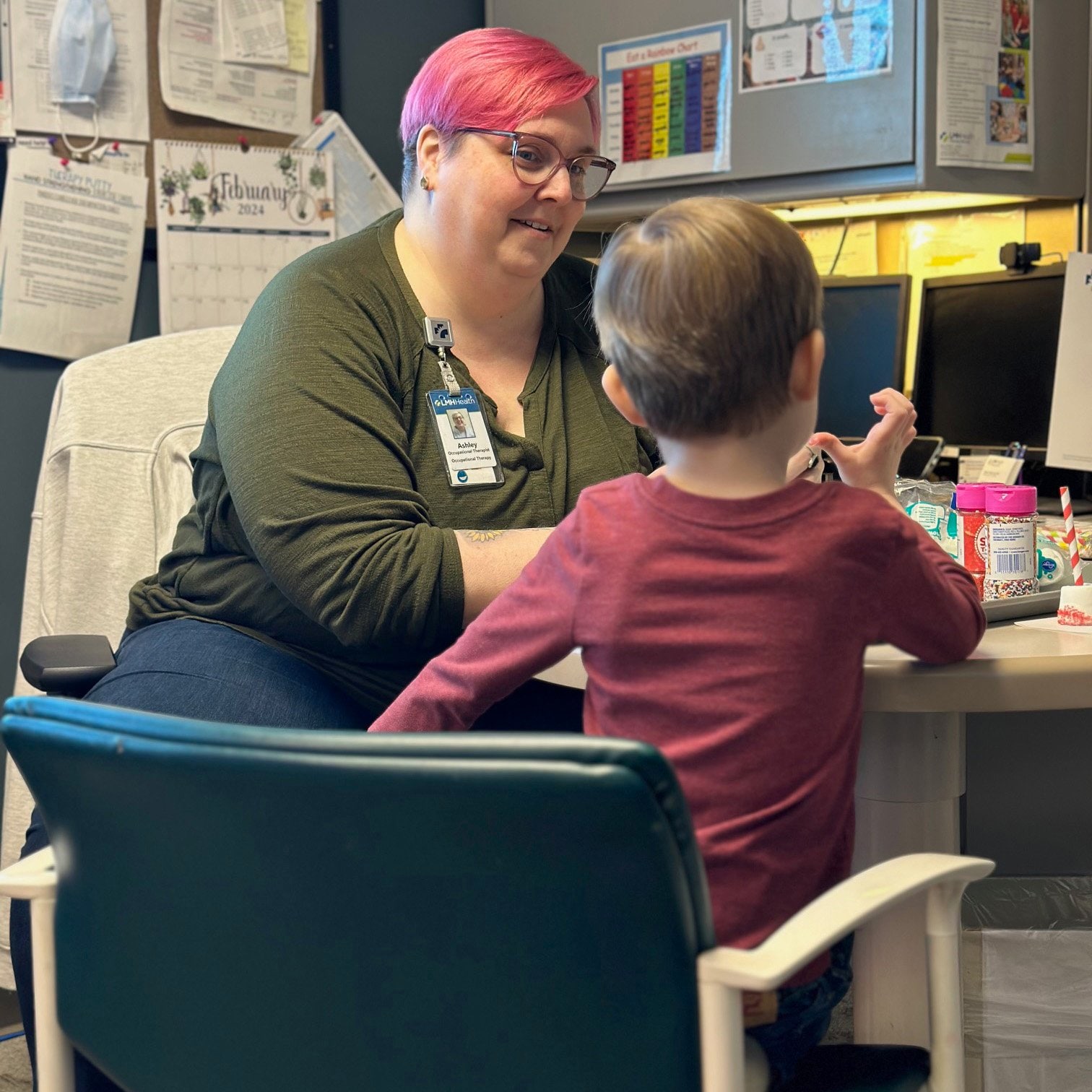
Ashley Miller and Zachary
You only have to flash back a couple of years to be surprised at the string of words erupting from this sweet little boy.
Zachary’s pregnancy wasn’t the easiest for his mom, Kathy. She’d had a couple of setbacks, including reduced activity, and knew that it was important to prevent early labor. Kathy knew he’d arrive early and had a C-section scheduled a month ahead of her due date.
“Dr. (Lynley) Holman delivered Zachary. I felt this confidence from her that I totally trusted, and I wanted to be in her hands for this,” Kathy said. “I felt like we were a team and had total confidence in her and LMH Health.”
Once Zachary was born, he wasn’t breathing well. His father, Patrick, stayed with Zachary as he was transferred to Overland Park Regional Medical Center for higher-level care, while Kathy stayed at LMH to recover from surgery.
“It was hard for me, but I wanted to be my best for Zachary,” she said. “When I was released from LMH, I lived at Overland Park for 15 days. I didn’t even go outside. I wanted to be there with him as much as I could be.”
Zachary spent two weeks in the NICU and was on oxygen, and the doctors told Kathy and Patrick to be prepared for the possibility that he may have developmental delays. As Zachary got older, he refused baby food and would only consume breast milk. He was on the lowest end of the growth scale, so Dr. Beth Rundquist, Zachary’s pediatrician, recommended an appointment for feeding therapy.
Will he ever do it?
The family turned to Karen Flory, a speech pathologist with LMH Health Therapy Services, for help when Zachary was 13 months old. Flory works with babies, both outpatients and inpatients at the hospital and is trained to work with fragile feeders, including premature babies and newborns.

Karen Flory
“I see a lot of babies for feeding difficulties. When they start solids, it can be a difficult transition for some,” she said. “It was that transition where Zachary began to have some issues.”
Flory shared that she works with a number of children like Zachary who are orally aversive, meaning they avoid foods of certain types and textures or sometimes don’t eat at all. She explained children with oral aversion don’t have the oral motor skills to eat a food and don’t know what happens when it goes into their mouth.
“I started working with Kathy to help Zachary become less aversive to anything around his mouth, creating positive experiences through play and oral sensory toys,” Flory said. “Kids learn through play, so we did a lot of sensory play with food, and Zachary started to experiment with tasting foods on his own. We were playing with Jell-O and pudding, driving cars through it, and pretty soon, he’d start putting it in his mouth himself.”
Zachary continued to work with Flory and progressed to the point where he was eating typically, so they discontinued therapy. But around age two, Kathy became concerned that Zachary was having speech delays.
“He was only grunting the word ‘go’ and I didn’t know what was going on,” she said. “There’s a list of the number of words you’re supposed to be able to speak at a certain age, and Zachary was nowhere near that.”
Flory stepped in again, this time providing speech therapy. Zachary wasn’t babbling like a toddler usually would, so she began by working with him on environmental sounds and early words.
“I make myself ‘big’ when we play, using fun words like ‘wow’ and ‘whoa’ that children can see and hear very easily,” she said. “One day, after lots of repetition, he began to say ‘go’ and I think his mom and I cried a little.”
Flory also used other methods with Zachary, including augmentative alternative communication (AAC), a term for any kind of communication that augments verbal communication. This includes gestures such as simple signs, as well as visual and tactile clues for sounds. Flory also incorporates speech-generating apps on iPads to help her patients make a connection between hearing a sound and saying a word.
“AAC can be both low and high-tech – anything from sign language or cards that have a sound written on them to speech-generating devices,” she explained. “We use AAC a lot with our early talkers. Research tells us that it helps kids become better verbal communicators, and some kids will always need to use AAC to communicate with others.”
It wasn’t long before Zachary’s words began to come out, and he’s now off the charts in the depth of his language.
“It seemed like it would be impossible, but I knew he was a fighter. He’s got thousands of words now,” Kathy said. “He has an IEP (Individualized Education Program) for speech fluency – that’s the spacing between words and the lifts in the voice. Karen ascribes it to a motor delay. The words are in there, it’s just a matter of getting them out.”
Motor skills, too

Zachary made marshmallow treats to share for Valentine's Day
Zachary’s IEP assessment looked at a number of areas, not just speech. That testing revealed that he was in the 5th percentile for fine motor skills, which are the movement and use of the hands and fingers, including reaching, grasping and pinching. Kathy talked with Flory and Dr. Rundquist, and they both recommended enrolling Zachary in occupational therapy with Ashley Miller.
Zachary began meeting with Miller in May 2023 to improve his motor skills and for help with sensory processing issues. Bath time had been a challenge because Zachary was terrified of water and would shriek when he got wet.
“His mom knew there was something off when he couldn’t tolerate going out in the rain, bathing or washing his hands. It just wasn’t typical,” Miller said. “It wasn’t just water, though. Zachary also didn’t like to get sticky or pick up food without a utensil.”
A child’s primary occupation is play, so as with Flory, play is also a staple in Miller’s work. On Valentine’s Day, she and Zachary worked on making sweet marshmallow treats during his session. Melting white chocolate in the microwave, cutting straws to push into the marshmallows before dipping them in the chocolate and then rolling them in sprinkles seems like play, but it all helps to improve Zachary’s motor and self-regulation skills and it’s a ton of fun.
“Zachary loves coming to therapy, whether it’s occupational therapy or speech. I don’t know that I’ve ever had a kid with sensory issues progress as quickly as he has,” Miller shared. “It’s not like healing a broken arm. Sensory issues, how they respond and how they improve are different for each child.”
Great support makes all the difference
Both Flory and Miller recognize that Zachary has another asset working in his favor – the love and support he receives from his family.
“Kathy has been a great advocate for him and has been very involved,” Miller said. “She asks questions, takes the education we share with her home, disseminates it to the family and is invested in Zachary reaching his goals.”
Flory agrees that much of the reason for Zachary’s success lies in his mom’s carryover of what she learns in therapy.
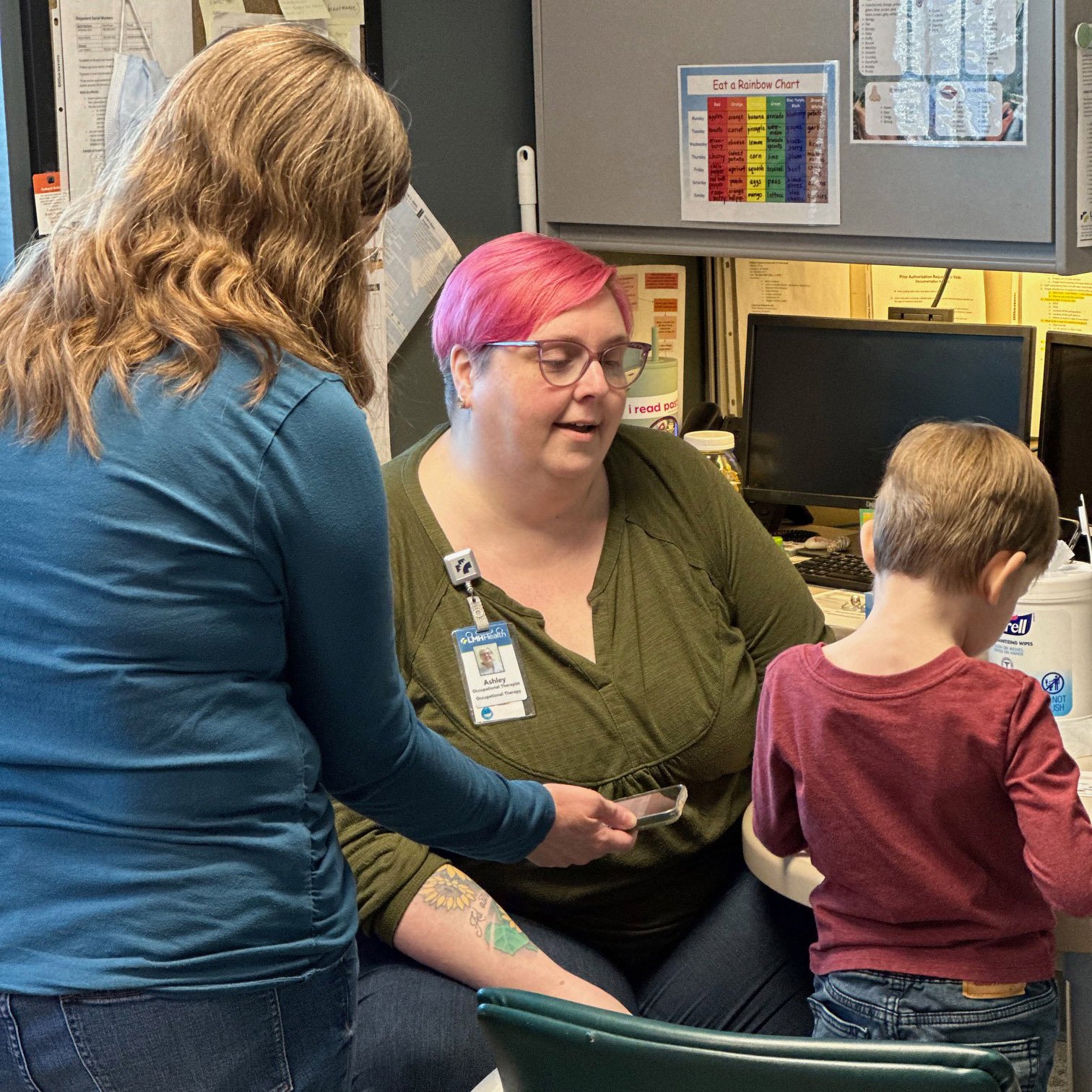
Kathy and Ashley discuss Zachary's progress
“The beauty of outpatient therapy is that we get to involve parents and caregivers and work together. Kathy takes it home and does it every day, with feeding, language and speech. I remember the day Zachary was making pizza with his mom. He spread on the sauce, put green peppers on it and decided to eat one,” she said. “He’ll eat so many more things now. Zachary has gone from a narrow palate to a wide one.”
Kathy knows that being actively involved in Zachary’s therapy has paid off in droves.
“You’ve got a golden window of time during the formative years, especially the first three, due to where they are with their brain development, where your kids can make the most progress with therapy,” Kathy said. “Be as engaged as you can be. Be in the room so you can see and learn what they’re doing and apply it throughout the week to maximize that therapy impact.”
If something’s off, what do I do?
If you notice that something is off with your child, Kathy suggests talking with their pediatrician. It’s important to be an advocate for their needs.
“I raised the flag and talked with Dr. Rundquist when I felt like something wasn’t quite right,” she said. “You might have to bring it up more than once, but it’s important that you’re heard.”
Zachary visits LMH Health Therapy Services weekly, working with Flory and Miller on alternating weeks. They work as a team to address Zachary’s needs and collaborate on care. This approach allows patients to receive multidisciplinary care in their own community and remain close to home. Kathy wouldn’t go anywhere else for care.
“Zachary truly looks forward to coming. If I say that we’re seeing Miss Ashley today, he squeals with delight,” she said with tears in her eyes. “He’s not nervous – he’s been comfortable with Ashley and Karen from day one.
“With them, you feel like you’re not just a number and you can tell they love what they do. I can’t imagine going anywhere else. They’re absolute rock stars.”