 Violence against healthcare workers rising
Violence against healthcare workers rising
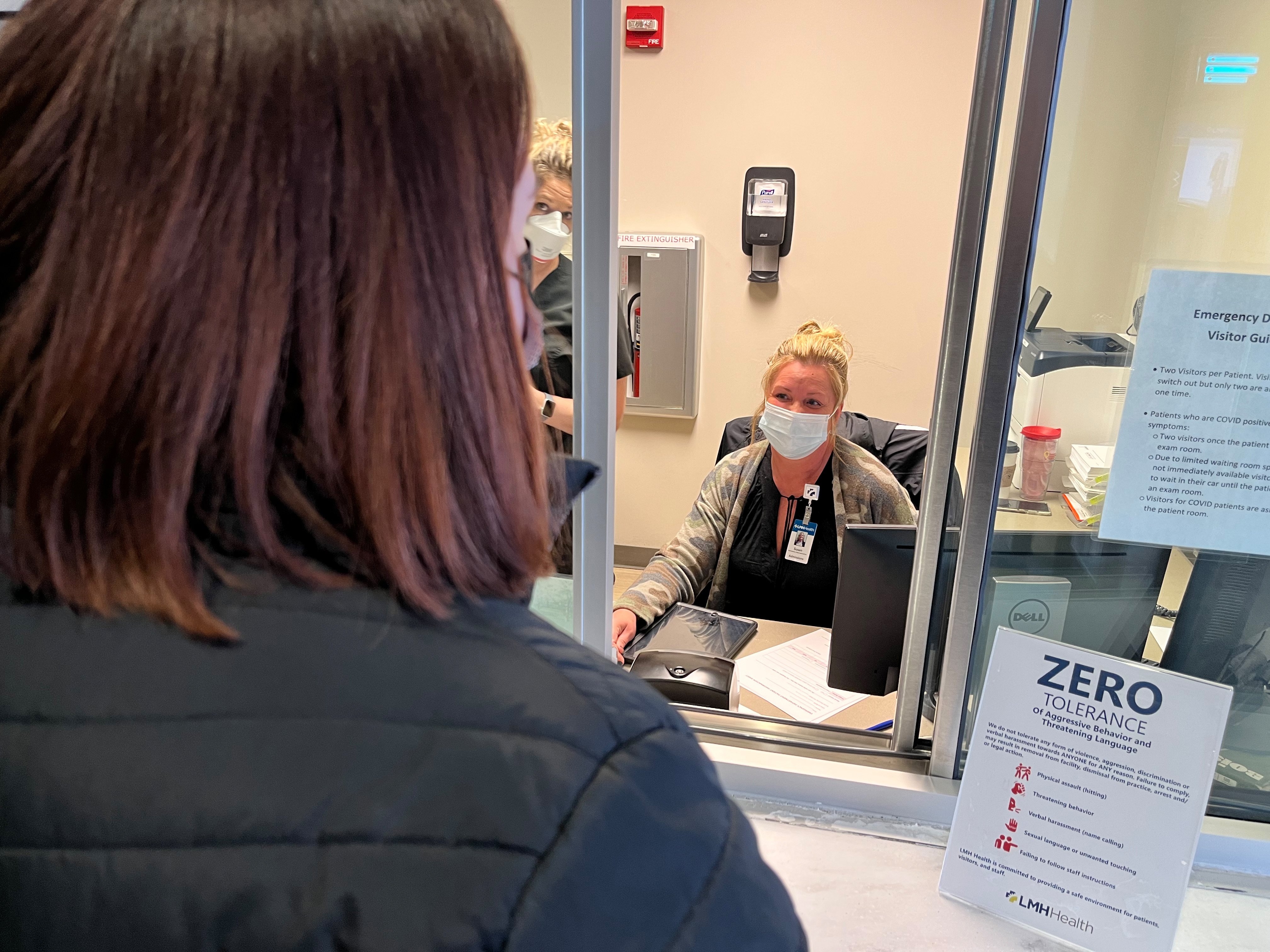
Needing healthcare in an emergency isn’t something that’s at the top of someone’s wish list. Faced with that prospect, patients and family members are scared, confused and not always sure which way to turn. That fear and anxiety can sometimes lead to violent behavior aimed at the very people that are there to help – healthcare workers.
“I think it would probably shock people in our community at the number of times our staff are the victims of violence in the emergency department setting,” said Jan Wiebe, LMH Health emergency department director.
Violent behavior doesn’t just include acts of physical violence, like spitting, scratching, hitting or kicking. We’re also talking about behavior that includes any act or threat of violence that occurs at the workplace or while an employee is doing their job. This includes threats of physical violence that cause an employee to fear for their physical safety and incidents where a firearm or other weapon is used.
“The majority of incidents we experience involve verbal assault, but there are incidents of physical assault as well,” said Rachel Haase, an emergency department charge nurse. “It primarily begins with nurses and aides because we’re at the bedside longer. Fortunately, our physicians and security staff are there to step in to help if things start to escalate.”
Facing the prospect of encountering violence on the job isn’t something that’s new to doctors, nurses and other healthcare workers. A 2018 report from the U.S. Bureau of Labor Statistics showed that three-quarters of all nonfatal workplace assaults and injuries occurred in healthcare settings.
“Violence against healthcare workers is something that’s underreported and the statistics confirm that,” said Danel Cupps, director for risk and compliance at LMH Health. “We know that it’s something that some staff just dismiss as part of the job.”
Cupps agreed that staff are on the receiving end of verbal assaults more often than experiencing physical violence. She said that patients who use vulgar language, yell at staff and call them inappropriate names is the chief complaint.
Protecting staff
Providing healthcare workers with the tools they need to contend with violent behavior is key to staying safe. LMH Health takes steps to reduce the likelihood of violence occurring.
Everyone in the organization is required to complete online de-escalation training each year - even those who don’t provide direct patient care. Staff in high-risk areas also undergo hands-on training, including those working in the emergency department, ICU and mother/baby unit, as well as others that request it.
“Having hands-on training gives staff the chance to learn about and practice maneuvers to get themselves out of physical situations,” Cupps said. “Learning what to do or how best to position yourself in a situation is key.”
If an incidence of violence does occur, staff are encouraged to report it – whether they’re on the receiving end or a witness – though violent acts are vastly underreported. A report from the Occupational Safety and Health Administration (OSHA) identified a healthcare worker’s professional and ethical duty to “do no harm” as one of the factors that may contribute to this practice. Other factors include:
- Feeling that experiencing violence is part of the job and being willing to put their health and safety at risk
- Recognizing that some injuries caused by patients are unintentional and therefore accepting them as routine or unavoidable
- Unwillingness to stigmatize perpetrators due to their illness or impairment
“The number one thing to do is to report any incident of violence that occurs at LMH. Having data about when, where and how incidents take place is key in making sure we have the information needed to address the behavior and to avoid the situation in the future,” Cupps explained. “We are committed to investigating each report and taking immediate and appropriate action against any individual, including staff, visitors and patients.”
Safety rounds
LMH Health senior leadership members began weekly safety rounds in January 2019, an activity designed to focus further attention on the safety of patients and staff. During safety rounds, which occur each week, members of the senior leadership team spend a few minutes talking with staff in each department at the hospital about safety and patient outcomes.
“Safety rounds have made it easier to report violent incidents and routine safety issues to senior leadership without concern. It’s also increased the speed in response time to those concerns,” said Traci Hoopingarner, chief nursing officer at LMH Health.
These rounds occur before the health system’s daily huddle, a time set aside each morning where staff members across the organization meet to talk about safety. The huddle provides an opportunity to share about safety issues occurring in other areas, providing space for staff to discuss potential safety barriers that may come their way.
“When safety concerns are shared with the larger group it also allows us to see if there are larger system issues at play. This is one of the ways we know that violence is an issue,” Hoopingarner said.
COVID adds extra stress to the system
Since the advent of the COVID-19 pandemic, healthcare workers across the nation have experienced an increase in violent acts. An ICU nurse in Jefferson Parish, Louisiana was attacked and knocked unconscious in January 2022 after an argument between family members escalated following the death of a relative.
“We hear about these occurrences and we’ve been fortunate that we haven’t had anything of this severity happen at LMH Health. Since the beginning of the pandemic we’ve had more incidences of violence across the organization, whether they’re due to the mask mandate, visitor policies or something else,” Cupps said. “Patients are angry that their families can’t come see them and for a while, we went through a period where people couldn’t see their loved ones at the end of life. All of this has compounded the anger and frustration.”
As critical care physicians, Amanda Gudgell, DO, and Krishna Rangarajan, MD, both are well versed in dealing with difficult and sometimes tense healthcare situations. They recognize that the ongoing pandemic has only increased the stress for patients and their families.
“The conversations we’re having are getting harder. There’s been a shift where there is a lot of distrust and anger,” Dr. Gudgell said.
While neither physician has been the victim of physical violence, there have been instances where they’ve been subjected to verbal abuse from families of patients being treated for COVID. They shared their frustration and sadness about the vitriol aimed at them.
“It makes me sad for us, for the nurses and everyone in the hospital working hard to try and help patients,” Dr. Rangarajan shared. “We’re trying to help people get through a time where they’re the sickest they’ve ever been. The distrust and anger – it hits you hard and it hurts.”
Dr. Gudgell shared the same sentiment. She wants people to remember that healthcare providers, whether they’re doctors, nurses, medical aides or staff, aren’t the enemy.
”We’re here to help you. We comb the literature and provide our patients with treatments that are beneficial. We’re tired of COVID too, but it’s not okay to take verbal abuse. We always hope it doesn’t escalate more than that,” she explained.
Longer wait times lead to frustration
Though masking requirements have caused some frustration, Haase said that’s not the issue cited most often in the emergency department – at least, not lately. That can be attributed to longer wait times resulting from higher numbers of patients seeking care and holding patients who need admission to the hospital in the emergency department until a bed becomes available.
“People are upset when they have to wait to be seen, but that’s the reality of where we’re at right now. Having a higher patient census means that you may have to wait longer for care,” she said. “When people are upset, frontline staff take the burden of that treatment.”
It’s also important to remember that when you come to the emergency department for care, you may not be seen in the order that you arrived. Patients are seen by a triage nurse to determine who needs to be seen first. Patients with potentially life-threatening illnesses or conditions, such as a stroke or heart attack, will be seen more quickly than those with less severe illnesses or injuries, like a sprained ankle.
Stressful conditions and the ongoing pandemic contribute to increased risk for aggressive behavior and violence toward healthcare workers, but LMH Health is committed to keeping staff, patients and visitors safe while they’re on any of our campuses.
“We continue to make progress,” Haase shared. “Creating an environment where staff feel empowered to share their safety concerns with senior leaders during weekly safety rounds is a great step in that direction.”